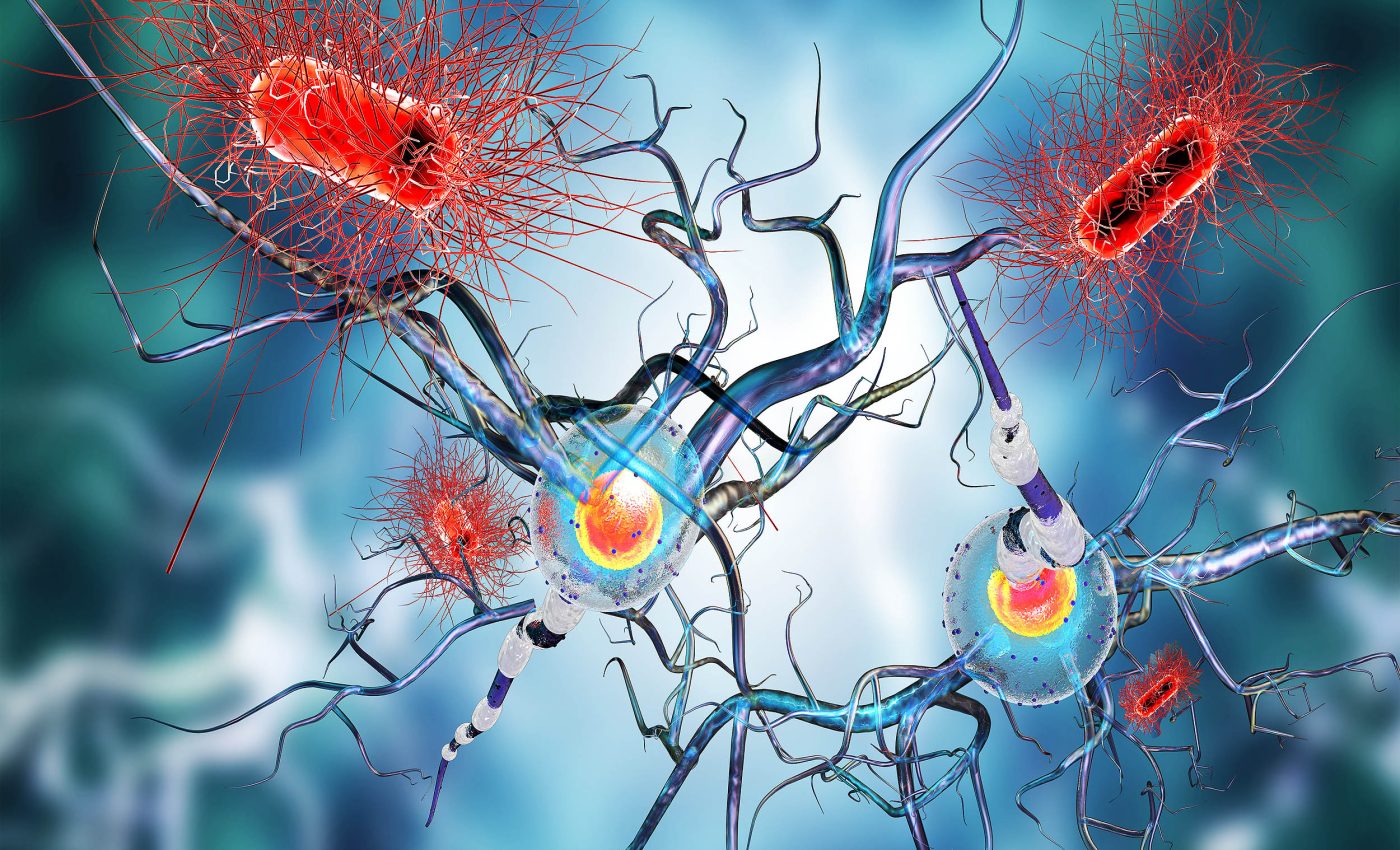
Scientists think they found two key bacteria that cause multiple sclerosis
For decades scientists have combed the gut looking for bacteria in the microbiome that push the immune system toward multiple sclerosis (MS). New evidence from a rare twin study now points a clear finger at two species of bacteria that hide in the small intestine.
The study, which compared 81 pairs of genetically identical siblings, singled out Eisenbergiella tayi and Lachnoclostridium as the most likely triggers of the nerve‑damaging disorder.
Dr. Anna Peters, who runs the lab in the Institute of Clinical Neuroimmunology of Ludwig Maximilian University of Munich (LMU) steered the international team that linked these bacteria to disease in both people and mice.
Tracing clues in identical twins
Identical twins share nearly every gene, so differences in health are often related to outside factors. By focusing on twins where only one sibling had MS, the researchers stripped away much genetic noise.
Detailed DNA tracking of gut samples revealed 51 microbial candidates whose numbers diverged between affected and unaffected siblings.
Two species of bacteria kept resurfacing with the highest odds ratios, putting them at the top of the watch list.
Those samples came from the ileum, the last stretch of small intestine that hosts a busy immune garrison. The choice mattered because pro‑inflammatory T cells gather here before they head for the brain and spinal cord.
A later comparison with the 1,152‑person International MS Microbiome Study echoed the same two species of bacteria. The overlap gave the Munich team confidence that their twin cohort was not a statistical fluke.
Gut bacteria linked to multiple sclerosis
To test cause rather than correlation, the investigators moved beyond sequencing. They transplanted ileal microbes from selected twins into germ‑free mice bred to develop MS‑like inflammation.
In animals that received bacteria from the sibling with multiple sclerosis, paralysis appeared within twelve weeks. Mice given microbes from the healthy twin stayed mobile the entire study.
Three female mice in one experiment showed a dramatic bloom of E. tayi just before MS symptoms set in. Their stool lost other common bacterial genera, hinting that the bloom crowded out potential competitors.
A follow‑up transfer from another twin pair repeated the outcome, this time with Lachnoclostridium dominating late in the trial. The signal again skewed toward female animals, matching the higher risk of MS seen in women.
Altogether, more than sixty percent of mice given “MS” bacteria developed spinal lesions, compared with fewer than ten percent in control groups. No other single species rose in step with disease across experiments.
Fiber-digesting bacteria and inflammation
E. tayi and Lachnoclostridium belong to the Lachnospiraceae family, a large clan of anaerobes that usually help digest fiber. Most relatives are considered harmless and even beneficial.
What sets these two apart is not yet clear, but the German group noted that both can thrive on mucus sugars when dietary fiber is scarce. That ability could thin the intestinal barrier and expose immune sensors to microbial products.
Earlier work on Akkermansia muciniphila showed a similar mucus‑eating habit that sometimes heightens inflammation. The new study hints the same mechanism may operate here but in a much smaller bacterial niche.
Another clue comes from metabolic profiling, which found that E. tayi produces ethanol and succinate, both known to stimulate Th17 immune cells. Excess Th17 activity drives attack on myelin, the insulating layer around nerves.
Why Lachnospiraceae may stir trouble
In a controlled ulcerative colitis model, certain Lachnospiraceae pushed macrophages toward an aggressive stance. Similar macrophage patterns emerged in the spinal cords of the colonized mice.
Other studies, however, have reported anti‑inflammatory roles for different members of the family, underscoring that taxonomy alone is not destiny. Context, gene content, and surrounding microbes all shape outcomes.
The twin study design hints that environment tilts the balance, because both siblings inherit the same immune genes. Diet, antibiotics, or viral history may give the two microbes the foothold they need.
“Together with our functional studies, this supports our conclusion that these bacteria might play a crucial role as environmental triggering factors of human multiple sclerosis,” wrote the researchers.
The statement marks one of the strongest causal claims yet made about the role of gut bacteria in the development of multiple sclerosis.
Multiple sclerosis bacteria treatment
Nearly one million Americans live with MS, and existing drugs only slow its progress. Targeting a pair of bacteria offers a simpler aim than re‑engineering the whole gut microbiome.
Researchers already use narrow antibiotics, phage cocktails, and engineered probiotics to chase single species in the gut. Similar tools could curb E. tayi or Lachnoclostridium before they spark immune trouble.
Another route involves adding fiber to keep mucus eaters occupied with safer food. Early trials of high‑propionate diets have shown modest symptom relief and could complement microbe‑directed therapies.
Limitations and next steps
Any multiple sclerosis therapy will also need to respect the wider community of gut bacteria that support vitamin synthesis and immune tolerance.
Removing the wrong microbial strains could backfire, as seen when broad antibiotics sometimes worsen autoimmune flares.
That risk has pushed researchers toward bacteriophages, viruses that hunt specific bacteria, which are already in early studies for inflammatory bowel disease.
A similar designer phage could trim the Lachnospiraceae culprits while leaving friendly neighbors untouched.
Regulators will demand hard proof that tweaking the microbiome alters biomarkers such as neurofilament light, a blood protein that rises when neurons die. The twin‑mouse pipeline described by Peters now offers a way to collect that evidence quickly.
Continued collaboration between neurologists, immunologists, and microbial ecologists will decide how quickly these insights can be turned into medicines.
For now, the results give patients a tangible target, and a fresh reason to care about what lives in their gut.
The study is published in PNAS.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













