Scientists learn that some genes are like a light switch and turn 'on' or 'off,' nothing in between
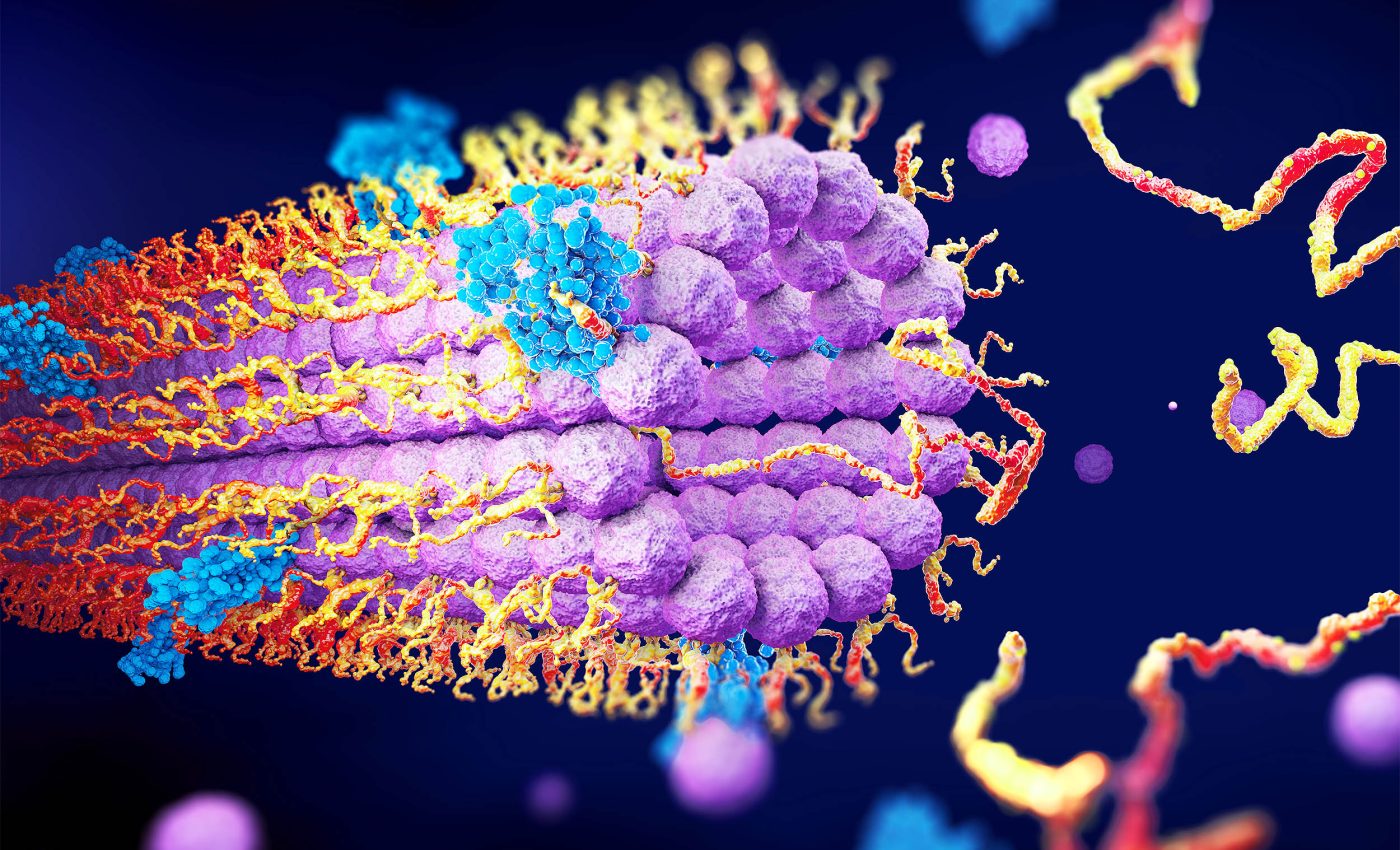
The machinery inside of each human cell usually behaves like a dimmer, turning genes up or down as needed. A new analysis shows that hundreds of human genes shun the dimmer and act more like a light switch, clicking fully on or off depending on the person.
The study was led by geneticist Omer Gokcumen at the University at Buffalo. His research reveals that this switch-like behavior may influence everything from fertility to cancer risk, depending on which genes are on or off.
Understanding genes – the basics
Genes are like the body’s instruction manual, written in a language made of DNA. They tell cells how to build proteins, which do all kinds of jobs – from carrying oxygen in your blood to helping you digest food.
Each gene is a stretch of DNA made up of four chemical letters (A, T, C, and G), and the order of those letters determines what kind of protein gets made.
It’s like a recipe: change one ingredient and you could end up with a different dish – or in this case, a different trait like curly hair instead of straight.
Things like diet, stress, or even pollution can switch certain genes on or off, without changing the DNA itself – this is what scientists call epigenetics.
So, even if you inherit a gene linked to a certain condition, it doesn’t always mean you’ll get it. That’s why twins with the same DNA can still turn out a little different.
The light-switch gene mystery
Early work on the lac operon in Escherichia coli proved that a gene can be either silent or roaring, nothing in between.
Researchers long assumed that such binary behavior was rare in humans because most traits need finer control. Yet the new report argues the opposite, showing that on‑off genes are widespread and often tied to illness.
Gene expression is simply the act of reading DNA and making proteins; most genes rise and fall smoothly. Switch‑like genes, by contrast, settle into either high or low camps, with few residents in the middle.
Hundreds of switch genes discovered
The team mined the Genotype‑Tissue Expression Project, a public atlas of 943 volunteers covering 27 tissues.
They applied a statistical “dip test” to 516,267 gene–tissue pairs and flagged 473 genes whose activity followed a crisp bimodal pattern.
“We believe switch‑like genes could one day be used to diagnose and perhaps even treat diseases,” said Gokcumen.
Only 40 of those genes showed on‑off states everywhere, implying hard‑wired DNA control, while the rest flipped only in certain organs.
Switch gene linked to health
Many of the 473 toggling genes sit at the heart of immune defense, metabolism, and cancer pathways.
Low expression of USP32P2, for instance, has been associated with male infertility, while off‑states in FAM106A may blunt the body’s response to COVID‑19.
Seven switch‑like genes in vaginal tissue, including ALOX12 and KRT1, shut down together in some women and correlate with vaginal atrophy, a postmenopausal thinning of the mucosa.
“This coordinated silencing hints at master switches we could eventually toggle therapeutically,” noted first author Alber Aqil.
Hormones switch genes on or off
The pattern of tissue‑specific switching pointed to hormones. In breast tissue, 157 of 158 switch‑like genes were far more active in women than in men, matching the estrogen-rich environment.
When systemic estrogen falls after menopause, the seven atrophy‑linked genes often flip off in the vagina, leaving the epithelium fragile.
About half of postmenopausal women experience symptoms of vaginal atrophy, yet most never seek help.
Epigenetics plays a role
Some switch-like genes are influenced not just by DNA or hormones but by DNA methylation, a chemical tag that turns genes off by altering how DNA is read.
In tissues like the breast and prostate, researchers found a strong negative correlation between gene expression and methylation at nearby CpG sites, which are common control points in the genome.
In the breast, for example, 71 switch-like genes showed this pattern, suggesting that epigenetic silencing explains why some people have these genes off.
That means two people with the same DNA sequence might express the gene differently depending on their epigenetic landscape, which can change over time due to age, stress, or environmental exposure.
Most switches are tissue‑specific
Out of the 473 switch-like genes identified, only a small group flipped on or off in every tissue. Most behaved like switches in just one or two types of tissue, such as the breast, colon, or vagina.
This tissue-specific pattern suggests that local conditions – like hormone levels or tissue-specific master regulators, control whether the switch flips.
Within each tissue, multiple switch-like genes tend to flip together, showing strong gene-to-gene co-expression. This clustering means they may be controlled by the same upstream signal.
For instance, in the breast, several genes turned on together in females and remained off in many males, reflecting the influence of estrogen on the tissue’s gene activity.
Switch genes aid diagnosis
On‑off states make ideal biomarkers because a simple assay can sort patients into yes‑or‑no categories. Topical estradiol, already used for atrophy, restores vaginal pH and thickens the lining by turning many of the same genes back on.
Universal switch‑like genes, often governed by structural variants, suggest another route: DNA testing could flag individuals whose deleted or silenced USP32P2 allele raises infertility risk.
The study argues that long‑read sequencing will uncover the missing structural variants and complete the binary map.
Beyond hormones, environmental exposures may tilt genetic switches, creating a fertile ground for gene‑environment studies.
Cataloging on‑off genes, the authors say, brings us closer to personalized medicine that treats the cause, not the symptom.
The study is published in the journal Nature Communications.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













