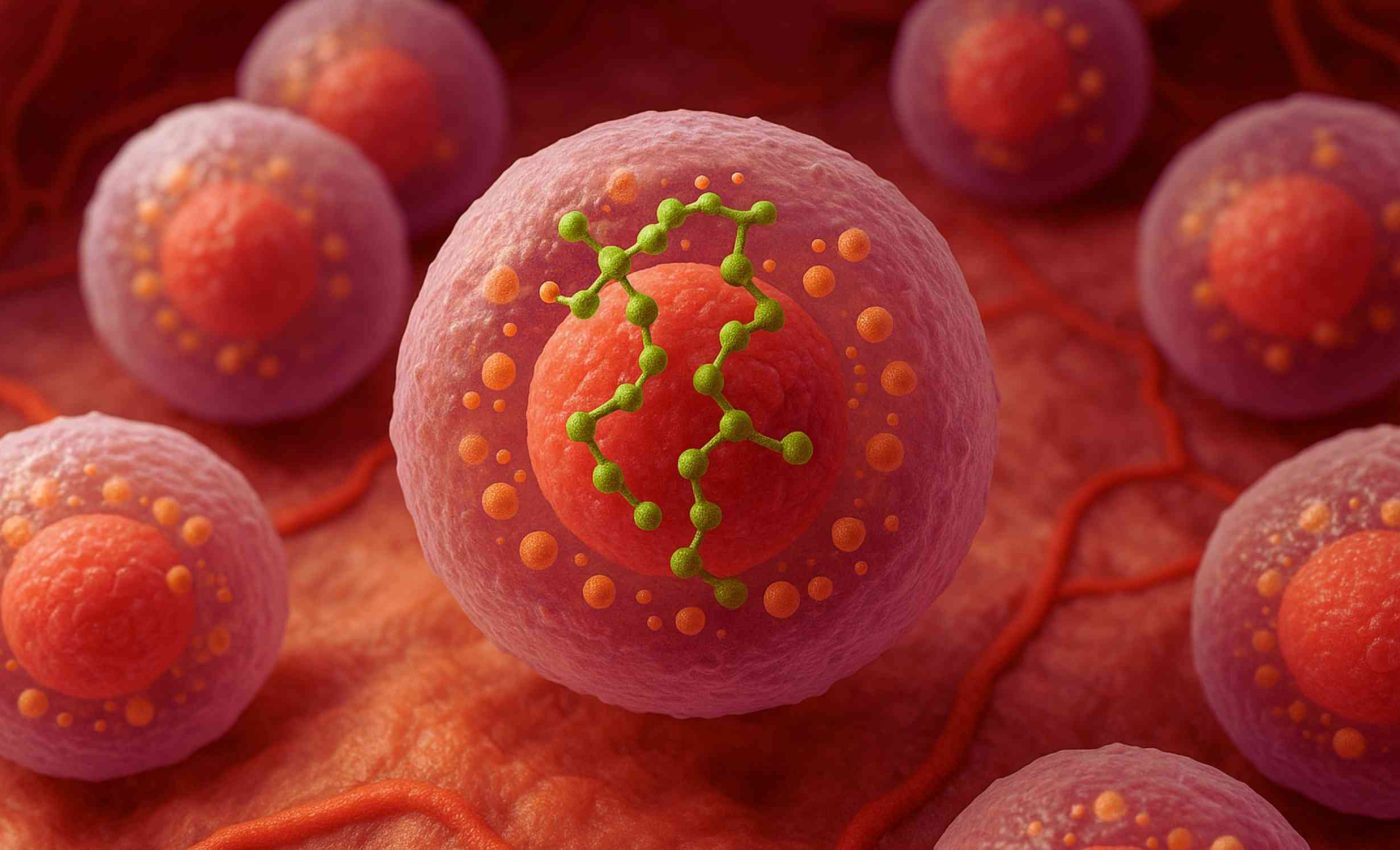
Scientists create tiny processors that function as 'circuits' inside human cells
Tiny engineered processors can now live inside human cells. These cell circuits work by passing a phosphate tag from one protein to the next, turning signals into action in a matter of seconds.
Xiaoyu Yang of Rice University led the effort, working with assistant professor Caleb Bashor and colleagues.
The team calls their invention a construction kit for synthetic sense‑and‑respond circuits that can sit quietly until disease markers appear and then release treatment.
Phosphorylation is the cell’s fast dial
Cells already rely on phosphorylation to race messages from the surface to the nucleus. Each tag adds a tiny negative charge that flips a protein between on and off, often in less than a minute.
Early synthetic biologists copied DNA logic instead because transcription is easier to program. Projects such as the bacterial repressilator showed that gene‑based loops can hum for hours, yet their slow pace limits medical use.
The Rice group chose the faster route. They treated every kinase–phosphatase pair as a Lego‑style block, then wired blocks together to build entirely new pathways.
Building cell circuits from protein
Yang and co‑workers designed substrate domains that do not exist in nature. They also built matching reader domains that bind only when a phosphate is present, ensuring clean input‑output links.
“Each module is independent, so we can tune one without breaking the rest,” explained Yang at the study launch. The modularity let the researchers stack up to four cycles without slowing the final response.
Previous attempts tried to graft synthetic parts onto native pathways, an approach that often misfired or drained cell energy. The new cell circuits run in parallel and leave natural signaling intact.
Cell circuits in humans
Because phosphate tags move fast, the synthetic networks respond to inflammatory cytokines within minutes. That is orders of magnitude quicker than transcription‑based drug switches that need several hours to make RNA.
In lab tests a single picomolar burst of tumor necrosis factor‑α triggered a clear fluorescent readout. The circuit then amplified the weak pulse into a thousand‑fold rise in output protein, matching predictions from quantitative models.
Many cancer therapies struggle with on‑target side effects such as cytokine release syndrome, which affects up to 100 percent of CAR‑T recipients in severe cases. A rapid shut‑off circuit could damp that storm before damage spreads to multiple organs.
Toward smarter therapies
Bashor’s group wired one synthetic cascade to a gene cassette that secretes interleukin‑10 (IL‑10), a well‑known anti‑inflammatory mediator.
When the engineered human T cells sensed an autoimmune flare signal in a dish, they released just enough IL‑10 to calm the response, then returned to standby.
“Programmable circuits let cells act only when and where they are needed,” noted Bashor after the first successful run. That precision opens doors to implantable therapies that do not rely on external pumps or repeated injections.
Other teams have used synthetic Notch receptors to shape T cell behavior, but those tools rely on protease cleavage and downstream gene activation that can take hours. The phosphorylation kit adds a faster layer that could sit upstream of existing control schemes.
One of the biggest advantages of phosphorylation circuits is their tunability. By adjusting the expression of each component, the team can fine-tune how strongly and how quickly a cell reacts to a given input.
This level of control is important in real-world settings where too much or too little activity can be harmful. A miscalibrated circuit could overstimulate the immune system or miss a critical disease cue, so every variable must be dialed in with care.
Cell circuits and the future
The Rice researchers now aim to test their kit in three‑dimensional tumor models. They also plan to explore how many cycles can be chained before noise overwhelms the signal.
A key hurdle is delivery. Lentiviral vectors work in the lab, yet clinical translation will need safer cargo trucks such as non‑integrating DNA or mRNA.
Regulators will likely ask how the circuits behave over months. Long‑term stability studies are therefore underway, including checks for unintended crosstalk with stress pathways.
Even with those caveats, the work shifts synthetic biology toward protein‑level control over mammalian physiology. It echoes early calls to treat living cells as programmable matter, but now at a speed that matches rapid disease dynamics.
The study is published in Science.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













