New twist boosts immunotherapy treatment in cancer patients
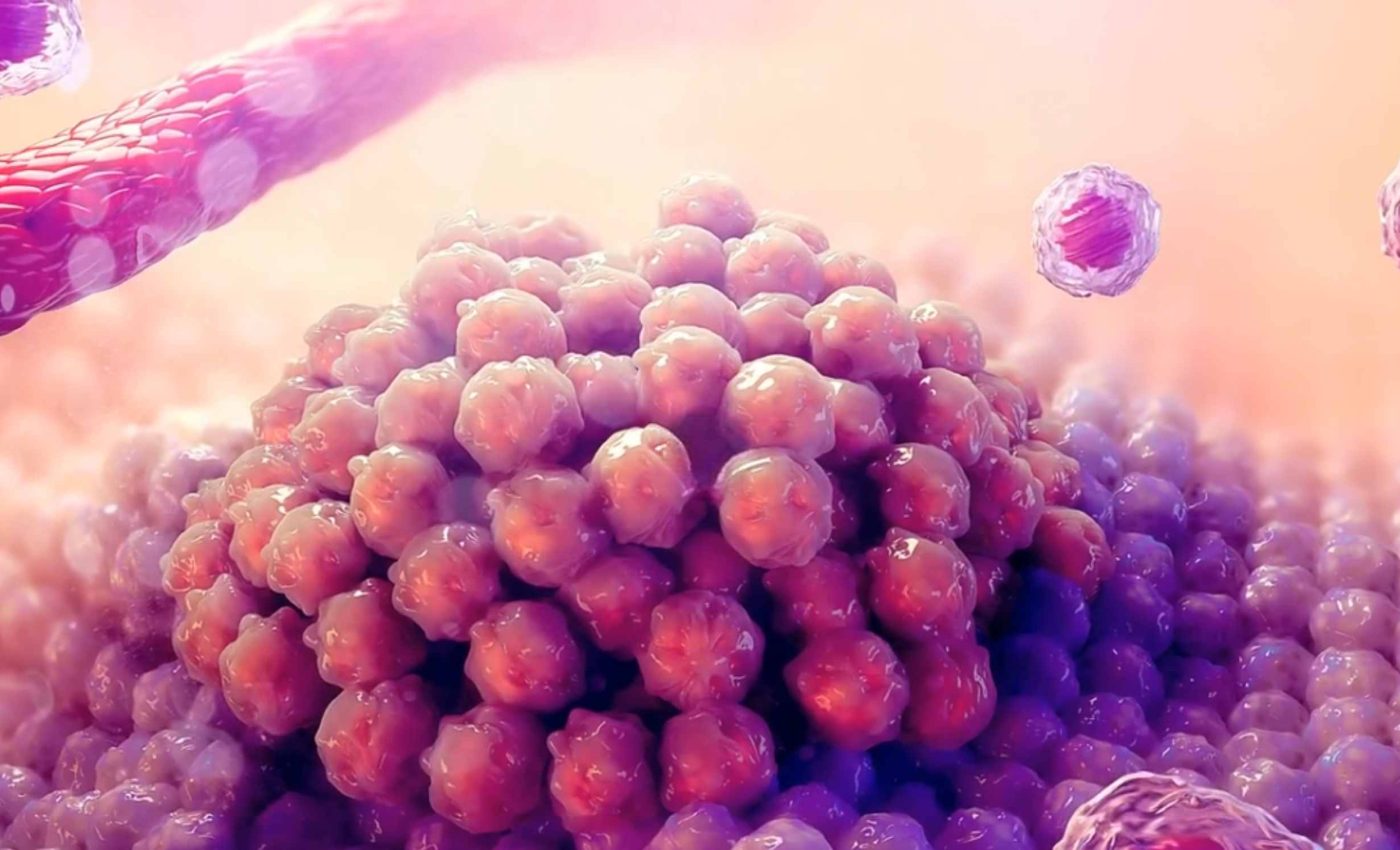
A new study explains why many tumors ignore immune boosting treatments. It points to a missing gene called MTAP and suggests that an older drug, DFMO, can switch a silenced alarm back on.
This STING (Stimulator of Interferon Genes) pathway is part of the body’s first line of defense and helps cells raise type I interferon signals when they encounter misplaced DNA.
Type I interferons are immune signaling proteins that alert nearby cells and activate antiviral and anticancer defenses. It acts like a sensor that detects fragments of DNA floating where they should not be, often a sign of infection or cancer.
STING and MTAP
Cells carry tools for cytosolic nucleic acid sensing, a defense system that detects bits of DNA or RNA floating in the cytosol, the fluid inside cells where genetic material normally does not appear.
When such material is found, it signals possible infection or cancer. When that alert is loud, immune cells can find tumors and act.
Trials with STING agonists have struggled to deliver in people. According to the Science editorial summary, results that looked promising in animal studies have so far failed to translate into success in human clinical trials.
Turning these alerts into real clinical benefit requires a clear signal inside the tumor. If that signal is weak, immune cells do not get the right cues.
The new work explains one reason the signal fails in many human cancers. It ties the failure to the loss of a single metabolic gene, MTAP.
Deletion that flips the switch
Across large patient cohorts, tumors with missing MTAP made up 8.9 percent in The Cancer Genome Atlas (TCGA) and 6.6 percent in GENIE. Rates are higher in certain cancers, which makes this deletion important in real clinics.
Research showed that when cells lose MTAP, a small molecule called methylthioadenosine starts to pile up. This buildup blocks another protein, PRMT5, which normally helps control how genes turn on and off.
As a result, a key immune signal called IRF3 drops, and the cell’s internal alarm system never fully activates.
MTAP loss does more than harm the cell that carries it. The excess metabolite can leak out and suppress PRMT5 in nearby cells that still have MTAP.
That spillover creates an immunosuppressive neighborhood. The tumor microenvironment ends up short on interferon signals and short on the immune traffic tumors need to shrink.
Reactivating a weak signal
DFMO blocks ornithine decarboxylase, an enzyme that helps make polyamines, small molecules cells use for growth and metabolism.
Reducing polyamines slows the buildup of methylthioadenosine, the compound that interferes with immune signaling.
With less of it around, the PRMT5 enzyme starts working normally again, IRF3 levels rise, and the cell’s ability to detect foreign DNA switches back on.
The drug is not just a lab tool, since the FDA approved oral eflornithine, also known as DFMO, in 2023 for high risk neuroblastoma maintenance therapy. Neuroblastoma is uncommon but serious. It strikes about 600 to 800 U.S. children each year.
The Science team used DFMO to lower methylthioadenosine, restore PRMT5 activity, and stabilize IRF3. In mouse models with MTAP deleted tumors, adding DFMO allowed STING agonists to work again.
STING, MTAP, and cancer care
MTAP status could guide immunotherapy choices. If a tumor keeps this gene, STING agonists may be enough, while MTAP deleted tumors might need a DFMO combination.
This approach adds a practical way to personalize care without inventing a brand new medicine. DFMO’s clinical use makes it easier to test combinations in well designed trials.
Clinicians could track interferon stimulated genes as early readouts of response. Clear signals in these genes would suggest the alarm is working again.
This strategy may also help explain past trial results. If many enrolled tumors lacked MTAP, the pathway may have been muted from the start.
What to watch next
Prospective trials must confirm that DFMO plus a STING agonist improves responses in MTAP deleted cancers. The Science report sets up the case for testing that idea in people.
Dosing and timing will matter. Giving DFMO long enough to drop polyamines and methylthioadenosine before a STING agonist may be key.
Biomarkers can help at every step. Measuring MTAP deletion and tracking interferon pathway activation could show who benefits and when.
Other options are in the queue. New PRMT5 targeted agents and metabolite lowering strategies might be paired with STING agonists if DFMO is not a fit.
The study is published in Science.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













