System that identifies and kills dying cells before they harm you has huge anti-aging potential
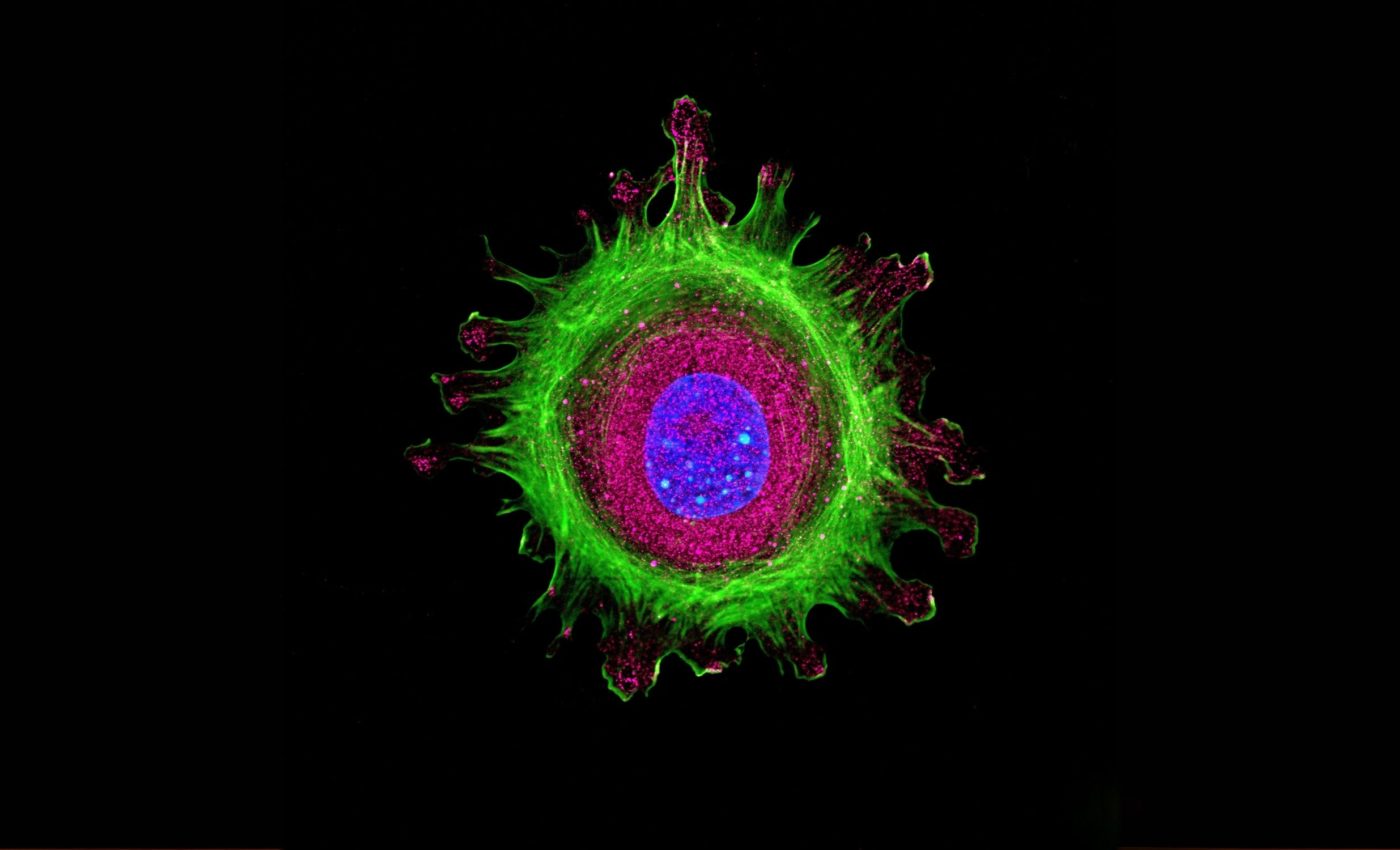
The human body ages one cell at a time. Most of those cells carry on with their jobs, but a small fraction slip into cellular senescence, a dormant state linked to arthritis, diabetes, and memory loss.
Assistant Professor Ippei Yagi and colleagues at Tokyo Metropolitan University say they can now spot those problem cells in seconds, and they never touch them with dye, antibodies, or enzymes.
Senescent cells cause damage
Senescent cells stop dividing, yet they refuse to die. They pump out proteins that stir up chronic inflammation, helping drive clogged arteries and brittle joints, according to a landmark 2011 Nature paper that removed such cells from mice and delayed several age‑related disorders.
Earlier work showed the same animals regained exercise capacity once the so‑called “zombie” cells were cleared, nudging drug developers toward senolytic compounds that wipe them out.
Clinical reviews now count more than a dozen early trials of senolytics like dasatinib and quercetin, though researchers caution that the field still needs larger studies to prove safety and dosing.
Before any pill can be approved, scientists must measure how many senescent cells a tissue holds and watch that number drop during treatment.
Most labs rely on fluorescent tags that bind to enzymes such as β‑galactosidase or to proteins like p16^INK4a.
Those markers work, yet the staining process can take hours and may alter the very cells under study. High‑throughput screens, tissue biopsies, and regenerative medicine all need a faster, gentler readout.
Electric fields reveal cell identity
Yagi’s team turned to frequency‑modulated dielectrophoresis (FM‑DEP), a method first described more than two decades ago for sorting live cells with microelectrodes.
When a non‑uniform alternating electric field washes over a cell, charges inside the membrane rearrange, creating a tiny dipole that moves toward or away from the nearest electrode.
The speed and direction of that motion depend on the field’s frequency. Plot the response curve and a single “cutoff” frequency emerges where the force flips sign.
Every cell type owns its own cutoff, wrote Ronald Pethig in a foundational 2010 review of dielectrophoresis. Yagi wondered if aging alone would shift a cell’s electrical fingerprint.
Senescent cells flip earlier
The group cultured human dermal fibroblasts, the workhorse cells that knit skin together.
Some cultures divided briskly, others were coaxed to senesce by repeated replication until they hit their Hayflick limit.
Applying FM‑DEP, the scientists swept the field from 100 kHz to 20 MHz and tracked each cell’s zig‑zag path under a microscope. Young fibroblasts reversed course near 2.8 MHz, while senescent siblings flipped at roughly 1.9 MHz.
“That 30 percent gap is wide enough to separate populations with a single voltage ramp. FM‑DEP is rapid, easy to apply, and label‑free,” explained Yagi. Because the assay runs in a sealed chip, it keeps the cells healthy for follow‑up experiments.
Aging changes cell membranes
The shift in cutoff stems from changes in lipid composition. As fibroblasts age, their membranes carry fewer unsaturated fats and pack more cholesterol, thickening the bilayer and slowing charge redistribution.
Those findings dovetail with earlier biochemical studies showing oxidized lipids build up in senescent membranes and stiffen the cell surface.
The altered dielectric constant caused by aging makes cells respond as if they were slightly larger, even though their physical size hardly changes.
DEP aficionados have used similar shifts to sort stem cells, T cells, and malaria‑infected red blood cells.
A 2024 microfluidic study even achieved DEP sorting at flow rates 100 times faster than earlier chips, hinting that industrial‑scale purging of senescent cells from stem‑cell grafts may be feasible.
Potential uses beyond the lab
FM‑DEP could screen senolytic drugs in vitro by counting senescent cells before and after treatment within the same droplet.
It might also grade the “biological age” of skin samples, tracking how diet, UV exposure, or cosmetics shift membrane profiles over time.
Regenerative medicine stands to gain because transplanted stem cells sometimes fall into senescence during expansion. Removing those laggards before implantation could improve wound healing and tissue integration.
Clinicians exploring plasma‑derived therapies or stem‑cell serums also need clean batches free of inflammatory senescent cells. A label‑free sorter that plugs straight into a production line would streamline quality control.
More testing and safety checks
Yagi’s data come from one fibroblast line, so the next step is to chart cutoff maps for other tissues, including muscle, fat, and neurons.
Each cell type owns its own membrane recipe, and disease can tweak that recipe long before senescence sets in.
Cross-talk with traditional markers will help validate FM‑DEP. For instance, cells sorted as “young” should show low β‑gal staining and minimal p16^INK4a expression, while those showing signs of aging ought to exhibit the opposite profile.
Researchers also want to know if drugs that rejuvenate mitochondria or dampen DNA damage can nudge the cutoff back toward youthful values. Such shifts would give pharmacologists a real‑time readout of treatment success.
Finally, safety studies must confirm that high‑frequency fields leave no latent harm. Recent on‑chip DEP reviews suggest the forces used are well within established safety margins for live cells.
The study is published in IEEE Sensors Journal.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













