Scientists identify a cellular 'switch' that could reverse type 2 diabetes
Type 2 diabetes has affected millions across the world, with countless people experiencing daily blood sugar fluctuations and other health complications. Many individuals struggle with insulin resistance, which makes blood glucose levels hard to manage.
Emily M. Walker, Ph.D, a research assistant professor of internal medicine at the University of Michigan, along with colleagues at Michigan Medicine, studied the root causes behind faulty energy production in mitochondria that ultimately affect insulin production, resulting in diabetes.
They reported that halting a stress response inside cells may restore normal function, paving the way for treatments that could help reverse this metabolic disorder.
Understanding mitochondria – the basics
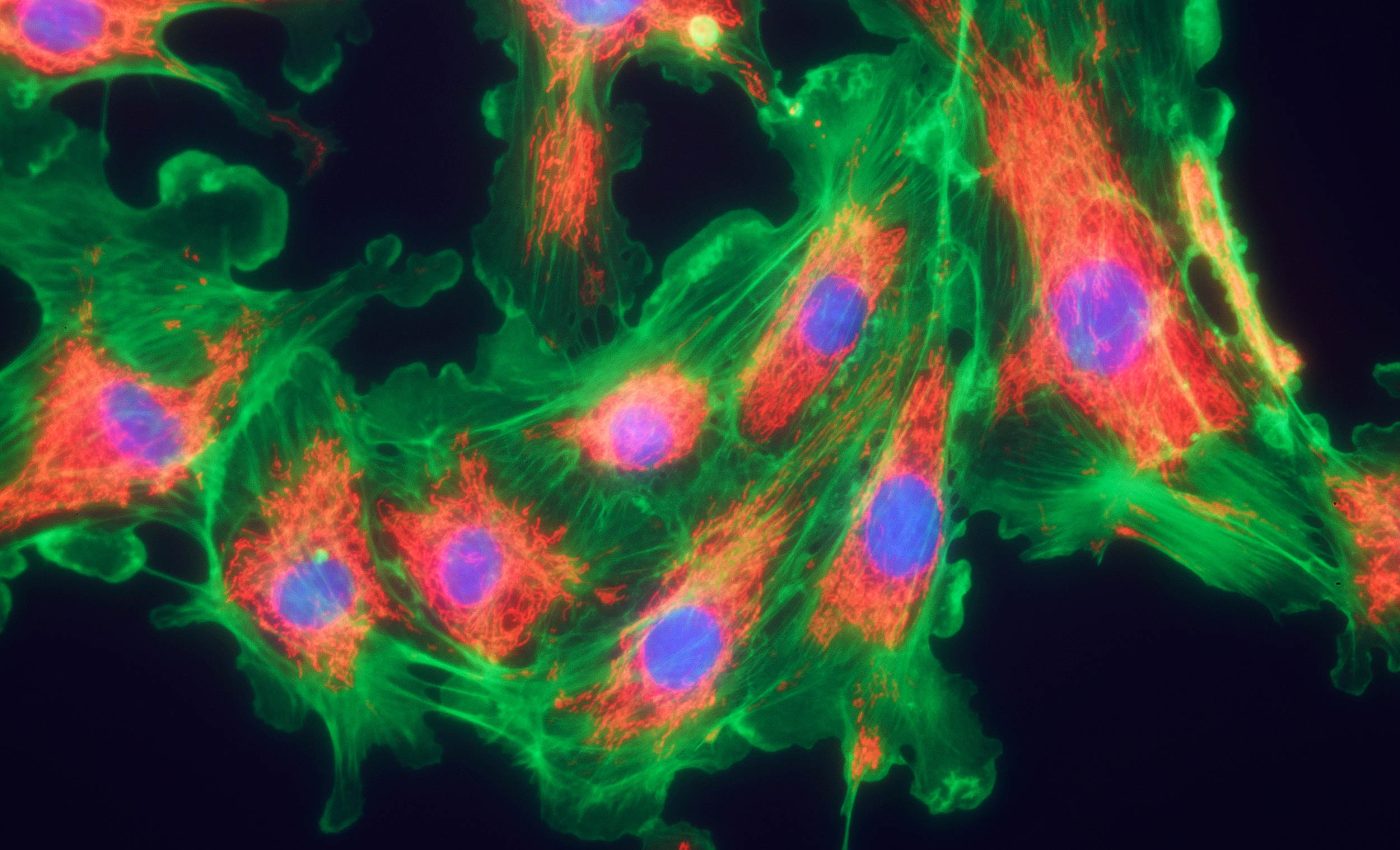
Mitochondria are essential organelles found in most eukaryotic cells, often referred to as the “powerhouses” of the cell. They generate adenosine triphosphate (ATP), the molecule that fuels nearly every cellular activity.
Beyond energy production, mitochondria also play crucial roles in regulating cell metabolism, calcium signaling, and even programmed cell death (apoptosis).
Structurally, mitochondria have a distinctive double-membrane design, with an outer membrane that encloses the organelle and a highly folded inner membrane that forms structures called cristae. These folds increase the surface area available for chemical reactions.
Mitochondria also possess their own DNA, which allows them to produce some of their own proteins and replicate independently of the cell’s nucleus.
Role of mitochondria in diabetes
Mitochondria hold a central spot in human biology because they convert nutrients into energy. When this conversion goes wrong, it can trigger a stress response that leads to poor insulin regulation and elevated blood sugar.
Many people with diabetes have experienced this shortfall, but the steps leading up to it were less defined until now.
“We wanted to determine which pathways are important for maintaining proper mitochondrial function,” said Walker.
The researchers identified a stress response that emerges from damaged mitochondria. By interrupting this stress response with a compound known as ISRIB, their results showed a marked improvement in blood sugar handling in mice.
Insulin-producing β-cells
A β-cell in the pancreas is responsible for releasing insulin, the hormone that regulates blood sugar.
These cells need high energy output from mitochondria to carry out their job. Weak energy conversion can disrupt insulin release, fueling the symptoms associated with type 2 diabetes.
Some earlier work pointed to mitochondrial problems in diabetic patients, but more clarity was needed.
The new observations suggest that damaged mitochondria trigger changes in gene activity, steering β-cells into a less mature condition.
Stressed mitochondria and diabetes
Investigators have also tested the same phenomenon in tissues like liver cells and brown adipocytes. The liver is a vital organ for glucose management, while brown adipocytes help regulate body temperature.
In each case, the same mitochondrial stress response emerged, pushing cells away from their main functions.
“We haven’t tested all possible cell types. Losing your β-cells is the most direct path to getting type 2 diabetes,” said Scott A. Soleimanpour, M.D., director of the Michigan Diabetes Research Center and senior author of the study. He noted the wide-ranging nature of diabetes in body systems.
Blocking the damaging stress response opens up intriguing therapeutic angles.
Restoring normal operation in cells that have not yet died offers a chance to shift type 2 diabetes management away from just mitigating symptoms. By preserving the identity of β-cells, the overall insulin balance can improve significantly.
Many drugs now in use either target blood sugar directly or boost insulin output. A drug that protects β-cells by hindering the cellular stress response could complement existing approaches and lead to fewer side effects.
Experts also continue to analyze how reversing cellular distress might apply to other chronic conditions that share similar mitochondrial problems.
Spotlight on daily management
While the study focused on laboratory models, findings that reestablish insulin production stand out in a field searching for long-term solutions.
Type 2 diabetes is heavily influenced by lifestyle choices, but some people still experience complications even with diet and exercise.
A pharmaceutical that turns back the clock on β-cell health may help individuals who have not had success with current treatments.
Mounting evidence shows that cellular energy mishaps are closely linked to insulin resistance. The body responds to irregular energy signals by reprogramming cells, which sets off a chain reaction.
Researchers now have a better handle on why metabolic tissues lose their maturity and how reversing that shift might stabilize blood sugar.
Next steps and future hopes
Efforts are underway to further map out the exact interactions between mitochondria and the nucleus. Learning how cells translate stress signals into changes in gene function could unearth additional treatment paths.
Scientists also plan to test ISRIB-like drugs in human tissue samples, aiming for more options in real-world clinical settings.
In-depth genetic analyses may shed light on the subtler triggers behind type 2 diabetes. Tests on how lifestyle factors and genetic predisposition interact with mitochondrial maintenance could expand the scope of these findings.
For many people, new insights on restoring healthier β-cell operation are a welcome boost to ongoing research.
Researchers behind this project are optimistic that therapies designed to preserve β-cell integrity may alter the direction of diabetes care.
By easing the damage to mitochondrial systems, those who struggle with type 2 diabetes may find their condition more manageable in the years ahead.
The study is published in Science.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













