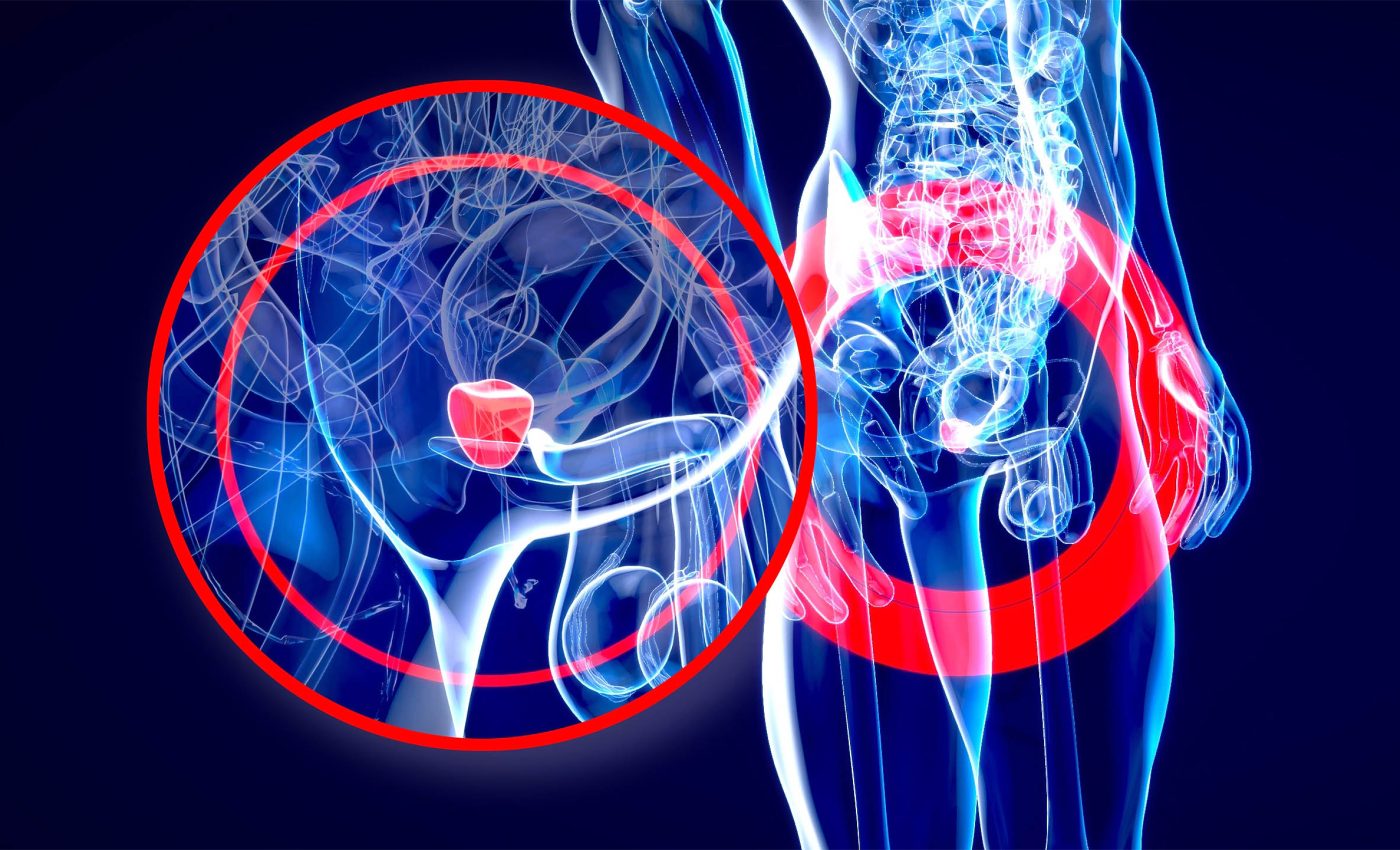
New drug combination slows progression of prostate cancer with BRCA mutations
An experimental drug pairing slowed the spread of advanced prostate cancer on scans in men whose tumors carry BRCA mutations.
In a large, international trial across 32 countries, adding niraparib to abiraterone and prednisone cut the risk of scan-defined progression by about half in that group.
What the trial tested
In the double blind, phase 3 international trial, 696 men with metastatic castration-sensitive prostate cancer – cancer that has spread but still responds to testosterone-lowering treatment – were assigned to the drug combination or to standard care.
All participants had changes in homologous recombination repair, a pathway that fixes broken DNA strands. More than half carried BRCA1 or BRCA2 changes, the group most likely to respond.
The trial was led by Gerhardt Attard at the Cancer Institute of University College London (UCL). Sites enrolled patients from multiple regions.
The study was registered before enrollment began. It used a prespecified plan to test results first in the BRCA group, then in all patients.
Lowering progression in BRCA group
In the BRCA group, radiographic progression-free survival was longer with the combination. The median was not reached for the combination versus 26 months with standard care.
In the full study population, the risk of scan-defined progression or death was lower with the combination. Time to symptom worsening also improved.
Radiographic progression-free survival – the time until scans show new or growing tumors or death – is a common endpoint in metastatic trials. Doctors rely on it to see benefit earlier than overall survival.
At the first look at overall survival, fewer patients had died than needed for a final answer. The trend favored the combination but did not yet reach statistical significance.
HRR gene changes
The biggest gains appeared in cancers with BRCA changes. In patients with other repair gene changes and no BRCA mutation, the effect was smaller and not clearly significant.
“Therefore, there is still a need for treatments that are tailored to patients whose tumors harbor HRR alterations,” said Attard.
About one in four men with metastatic prostate cancer carry HRR gene changes that can shape treatment. This group tends to have faster growing disease.
The results support routine testing for these DNA repair genes at diagnosis of metastatic disease. Early identification helps direct patients to therapies that match tumor biology.
BRCA drug combinations
Niraparib belongs to a class of drugs known as PARP inhibitors. These are medicines that prevent cancer cells from repairing broken DNA.
When a tumor cell already carries a defective BRCA gene, blocking PARP makes it harder for that cell to survive.
Abiraterone, on the other hand, shuts down androgen synthesis, the hormone pathway that fuels prostate cancer growth.
Together, they attack the disease on two fronts: one stops the cancer from fixing its DNA, while the other deprives it of hormonal energy.
Safety signals and tradeoffs
Serious side effects were more common with the combination than with standard care. Most were expected for these drugs and were manageable with dose changes.
Anemia and high blood pressure were the most frequent severe problems. About one quarter of patients on the combination needed a blood transfusion.
A small number of patients had rare events, including one case of myelodysplastic syndrome. Investigators will continue long-term safety follow up.
An FDA label for a niraparib plus abiraterone tablet used in resistant disease lists similar risks. That label also highlights the need to watch blood counts and blood pressure.
Why genes like BRCA matter
PARP inhibitor, a drug that blocks a DNA repair enzyme, can turn a tumor’s genetic weakness into a treatment target. Cancer cells that lack reliable repair may be pushed beyond their limits.
Back in 2005, scientists showed that BRCA-deficient cells are highly vulnerable to PARP blockade through synthetic lethality. Normal tissues remain less affected because they retain backup repair.
Blocking the androgen receptor pathway with abiraterone stresses prostate tumors in a different way. Combining both approaches may leave BRCA-mutant cancers with too few repair options.
Hazard ratio, a measure of risk over time, helps compare groups in a trial. A value near 0.5 in the BRCA group means about half the risk of progression compared with standard care.
What comes next
Researchers plan the final overall survival analysis when enough events occur. They will also explore which non-BRCA genes, if any, show clear benefit.
Many patients in the control arm received later therapies, including PARP inhibitors and chemotherapy. Real world treatment sequences will matter for how this combination is used.
For now, the data suggest that starting PARP inhibition earlier may help men whose cancer still responds to hormone lowering. That is a shift from using these drugs only after resistance develops.
The study is published in Nature Medicine.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













